Today I am providing a summary of the Brain Health Report – Time matters in multiple sclerosis, which was last updated in 2018. Even though some new findings have been added since then, such as the importance of EBV infection and new therapeutic options becoming available, the core messages remain. These include the importance of early treatment, leading a brain-healthy lifestyle, seeing an MS specialist and making decisions about the treatment of your condition together with your neurologist. Because only those who stand behind their decisions will stick to them in the long term. Also, the fact that cognitive impairment contributes significantly to a reduced quality of life and has a significant impact on whether a person with MS can continue to work full-time or at least with reduced hours. I have tried to summarize the most important key messages in easy-to-understand terms.
Klicken Sie auf den unteren Button, um den Podcast zu laden.
Table of Contents
All graphics used are taken from the aforementioned presentation. You will also find all the references for the individual statements in the original file. I have omitted them here and left only the core statements. This has made the text easier to read 😉
You can find more valuable information on the website www.msbrainhealth.org.
Brain health. Time matters in multiple sclerosis
Last updated 22 August 2018
As mentioned before, the knowledge has increased in the last five years with new therapeutic options on the horizon, new biomarkers, and even stronger approach to flipping the pyramid of treatment. This means starting of therapy with a strong medication that suppresses the inflammation effectively and tries to decrease neurodegeneration. Nevertheless, this report contains many useful facts that are still valid today.
The ultimate goal is to keep the brain as healthy as possible at all stages of MS. All statements and recommendations keep coming back to this point. The focus is on rapid diagnosis and constant monitoring of MS as it progresses. This includes monitoring the therapy. Because if it does not work, the disease-modifying therapy should be changed. In addition, more data should be collected to ensure that treatment is continuously improved.
Authors:
- Professor Gavin Giovannoni (Chair), London, UK
- Professor Helmut Butzkueven, Parkville, VIC, Australia
- Professor Suhayl Dhib-Jalbut, New Brunswick, NJ, USA
- Professor Jeremy Hobart, Plymouth, UK
- Dr Gisela Kobelt, Mulhouse, France
- Mr George Pepper, Leeds, UK
- Dr Maria Pia Sormani, Genoa, Italy
- Mr Christoph Thalheim, Brussels, Belgium
- Professor Anthony Traboulsee, Vancouver, BC, Canada
- Professor Timothy Vollmer, Aurora, CO, USA
A total of 49 professional societies and interest groups worldwide support and endorse the contents and recommendations of the report (as of August 2018).

A look at brain health in MS shows that time plays a crucial role.
This is because disease activity can persist even if there are no symptoms.
It is extremely important that the neurological reserve is preserved.
It has now been proven that cognitive impairment has a practical impact. They even serve as an early indicator and predict the progression of physical disability.
If disease activity persists, damage occurs throughout the central nervous system (CNS).
In relapsing-remitting MS, it is assumed that the damage to the CNS is not limited to individual areas of inflammation. Rather, the damage is diffuse and persists throughout the course of the disease. The damage occurs in the white and gray matter.
In addition, accelerated brain atrophy (loss of brain volume) progresses throughout the course of the disease. It can even be observed in people with radiologically isolated syndrome (RIS) and clinically isolated syndrome (CIS).
Note: If disease activity continues, brain atrophy is accelerated.
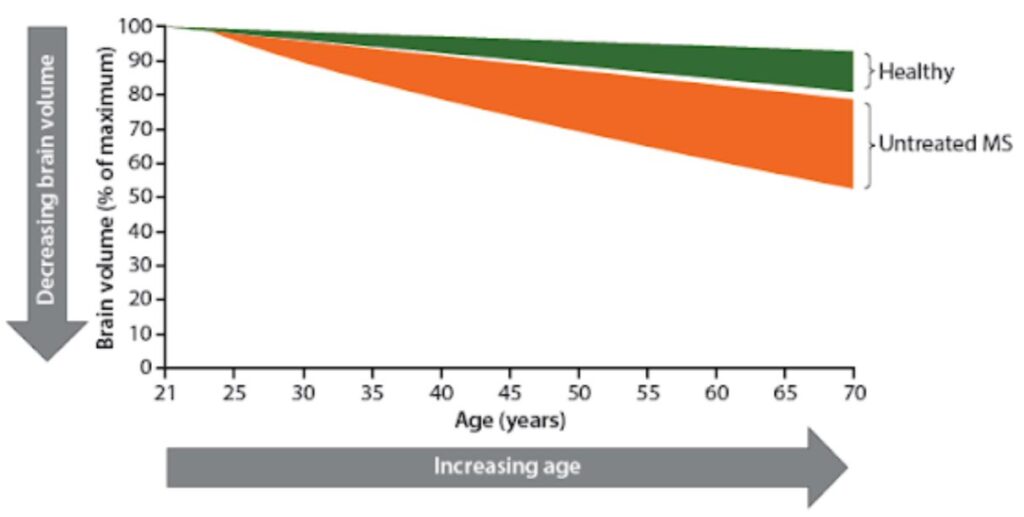
This example shows how the brain volume of a person with untreated MS decreases faster than it would be typical for a person’s age.
At the onset of the disease at the age of 25, the brain volume is still the same, but then decreases faster in an MS patient without treatment than in a healthy person.
Disease activity persists, but as a rule of thumb only one in ten lesions leads to a relapse.
On average, only one in ten lesions leads to a relapse. Nevertheless, every single lesion contributes to the loss of neurological reserve.
Monthly MRI examinations of seven people with relapsing-remitting MS (RRMS) over 1 year showed that the majority of disease activity is subclinical (not externally visible). A total of 50 new contrast-enhancing lesions were discovered in six of the seven MS patients examined. However, relapses occurred in only three of the seven patients. There were a total of five relapses.
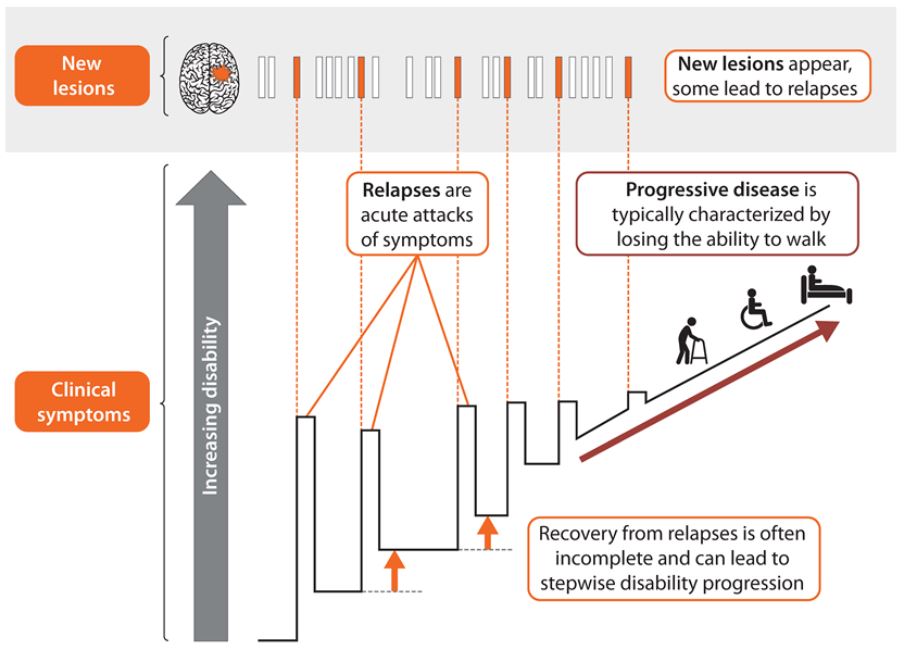
Note: The neurological reserve is finite and must be preserved as much as possible.
Neurological reserve is the limited ability of the brain to maintain its function by remodeling itself to compensate for the loss of nerve cells and fibers.

The neurological reserve may explain why MS-related brain damage remains undetected in the early stages of the disease. Unfortunately, this often leads to MS remaining undetected and untreated for a long time.
The neurological reserve must be preserved. It protects against progressive disability.
Preserving brain volume and cognitive reserve protects against increasing disability.
A brain volume meta-analysis of 13 randomized controlled trials involving more than 13,500 patients with RRMS showed that effective treatment leads to less disability and less loss of brain volume.
In addition, successful treatment resulted in less disability progression and fewer new and less enlarged MRI lesions.
A follow-up study on cognitive reserve with 859 MS patients revealed that patients with high cognitive reserve had a lower symptom burden than patients with low cognitive reserve.
Cognitive impairments have practical consequences.
Cognitive impairment in the early stages of MS is associated with the following factors:
- Reduced quality of life
- Reduced ability to cope with everyday life
- Reduced employability (The unemployment rate for people with MS is higher than in the general population, even with minor physical disabilities).
Note: Even if a person with MS is fully mobile most of the time, their employability is reduced. This suggests that cognitive impairment plays an important role.
Cognitive impairment predicts progression of disability.
Cognitive impairment can occur years before obvious clinical symptoms of MS.
A case-control study found that the academic performance of 75 people who later developed clinical symptoms of MS (84% RRMS; 15% SPMS; 1% PPMS) was worse than that of 75 people who did not develop MS. [Note: RRMS = relapsing-remitting MS, SPMS = secondary progressive MS, PPMS = primary progressive MS]
Cognitive function is an early indicator of short-term and long-term progression of clinical disability in patients with RRMS.
In a study on the short-term progression of clinical disability, 1,582 people with RRMS who were treated with placebo were observed for up to 2 years. It was found that baseline cognitive function predicted the progression of clinical disability. This was assessed using the following criteria:
- EDSS (Expanded Disability Status Scale)
- Multiple Sclerosis Functional Composite – a performance scale developed by the US National Multiple Sclerosis Society (NMSS) to assess the severity of disability in multiple sclerosis patients. A further development of the EDSS. The time required to cover a certain walking distance, a pin test to assess arm function and the assessment of cognitive functions were integrated as new components.
- Visual function test
155 people with RRMS who received treatment were examined in a retrospective study to measure the progression of clinical disability. After 10 years, there were clear differences between patients with fully preserved cognitive abilities at the time of diagnosis and those who already had cognitive impairment.
People with cognitive impairment at diagnosis were more than three times as likely to have an EDSS score of 4.0. They were also more than twice as likely to develop secondary progressive MS.
Three key recommendations for changes in treatment

1. Minimize delays in diagnosis and treatment
People with suspected MS should be referred immediately to a neurologist specializing in MS. This can speed up the diagnosis. The latest recognized diagnostic criteria should be used to diagnose MS as early as possible and start treatment quickly.
MS neurologists and clinics have specialized staff and equipment, which enables rapid diagnosis. In addition, MS nurses are better able to support patients. The care provided by MS specialists increases the likelihood that patients will take disease-modifying therapies. In addition, MS neurologists are familiar with rapidly evolving treatment options.
Furthermore, a multidisciplinary team provides an integrated approach to care in which different aspects of the disease are treated by different specialists.
It often takes up to two years between the first symptom and seeing a neurologist. A lot of time. There is a correlation between the delay in referral to a neurologist specializing in MS and the degree of disability at the time of the first visit.
Note: The longer the delay, the higher the initial degree of disability.
It is important that the latest recognized diagnostic criteria are used. Initially, the Poser criteria were used in 1984, which only included visible symptoms. Since 2001, the McDonald criteria have been used, which were adapted again in 2005, 2010, and 2017.
To illustrate, using the McDonald criteria (2001) instead of the Poser criteria doubles or triples the number of people diagnosed with MS within a year of their first attack.
Unfortunately, there are still regions of the world where prescribing guidelines require two clinical relapses before a DMT is initiated.
For people diagnosed with clinically isolated syndrome (CIS), treatment with a disease-modifying therapy (DMT) prolongs the time to a second relapse (i.e. progression to relapsing-remitting MS by all diagnostic criteria) and improves MRI results.
In people with clinically isolated syndrome or relapsing-remitting MS, early initiation of DMT treatment is associated with better long-term outcomes than delayed treatment.
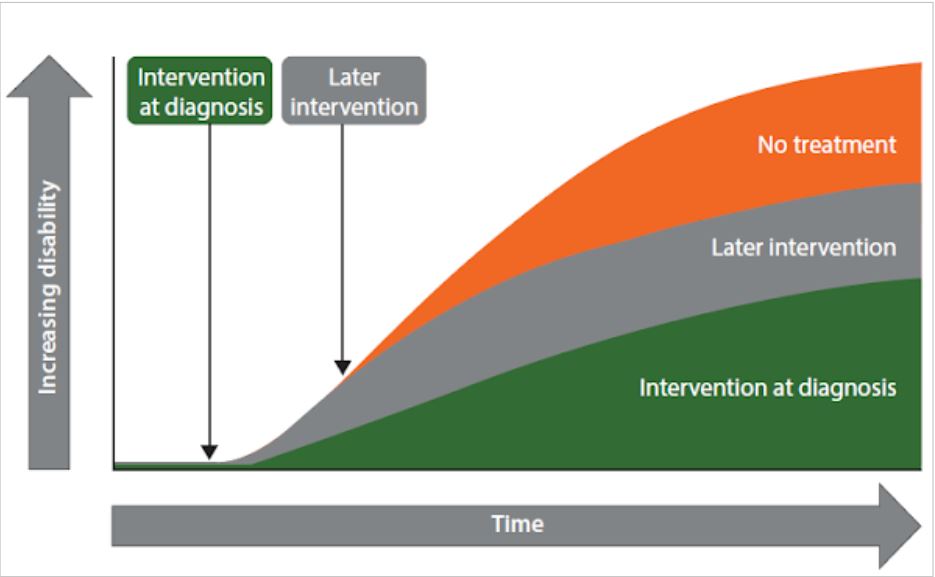
Overview of the key recommendations
The central recommendation is very clear: MS should be diagnosed and treatment started as soon as possible. Delays must be kept to a minimum, as these can lead to irreversible progression of the disability.

2. Monitor disease activity and provide targeted treatment
The treatment strategy should be a shared decision, i.e. doctor and patient discuss together how to proceed and agree on the next step(s).
The doctor should also encourage the patient to adopt a brain-healthy lifestyle. Each patient should have the full range of disease-modifying therapies to choose from, so that the most appropriate one can be selected.
The visible and invisible indicators of disease activity must be monitored and evaluated. If a medication does not achieve optimal treatment success, a change should be considered.
Shared decision-making
For shared decision-making, it is important to set an explicit treatment goal and proactively involve the MS patient in the decision-making process.
This involves empowering the patient with full knowledge of their situation so that they can make informed decisions about their treatment. The principles and benefits of a brain-healthy lifestyle are one aspect. The benefits of early treatment with agents that can alter the course of the disease is another. Possible consequences of inadequate or suboptimal treatment are a third.
MS patients who are well informed about their disease and its treatment and who build good relationships with their care team have a higher adherence to treatment. Adherence to disease-modifying therapy is associated with fewer relapses and lower medical costs.
A brain-healthy lifestyle
A brain-healthy lifestyle involves increasing activities that improve cognitive reserve. Patients can do this by increasing their cardiovascular fitness, consuming less alcohol, smoking less and preventing vitamin D deficiency.
In addition, comorbidities should be better controlled to reduce their negative impact on the progression of MS and limit the risk of non-MS related disability.
Availability of the full range of DMTs
The real-world evidence studies are carried out after the drugs have been approved in order to test their long-term efficacy.
The results on established DMTs are inconsistent. Most studies report that a particular class of established DMTs can slow (but not prevent) disability progression; others report no effect on disability progression. Others were only compared with placebo.
Explanation:
Established DMTs: A group of DMTs for relapsing forms of MS that were mainly approved in the 1990s, as well as reformulations and generic versions of these substances.
Newer DMTs: A group of DMTs approved for relapsing forms of MS after the 1990s, with approval conditions that differ from those of established DMTs.
Choose the most suitable treatment for your individual needs
Initially, the full range of DMTs should be available for people with active relapsing forms of MS, regardless of previous treatment. This helps to start the most appropriate treatment quickly, optimize efficacy and safety for each individual, and make a shared decision about the DMT that best suits each patient’s disease progression, values, needs, limitations and lifestyle.
Monitoring of clinical and subclinical indicators
Meta-analyses provide clear evidence that effective therapy influences all relevant factors in the course of the disease.
Patients with effective therapy have fewer relapses, fewer new or active MRI lesions and lose less brain volume.

Evaluation of all parameters
To assess disease activity, all parameters that predict future relapses and disability progression must be included. Over the years, assessments are constantly updated as new scientific findings emerge.
An important component is MRI brain scans at set intervals and when needed to monitor lesions and brain volume loss.

In general, MS patients should be treated with a disease modifying therapy for as long as there is a risk of inflammatory disease activity in the absence of treatment.
A change of therapy should be considered if the treatment is not responding optimally. Clear principles for recognizing treatment failure are needed to make this decision meaningfully.
Overview of the key recommendations
Key recommendation: Set goals for treatment and ongoing management that aim for the best possible outcome for each MS patient.

3. Development and use of robust evidence
The aim is to gain and use knowledge from everyday treatment based on a broad and long-term database in order to continuously improve decision-making. This is the only way that treating physicians can draw on sound knowledge.
To achieve this, data must be proactively collected and recorded using standardized data collection techniques and protocols. This data can and should be used in daily practice. By integrating anonymized, standardized and comparable data into national and international registries and databases, new knowledge can be gained and used more quickly.
Regulatory authorities, health technology assessment bodies and payers need to make initial decisions about DMTs based on data from short-term clinical trials. Recent real-world evidence on the long-term efficacy and safety of DMTs is needed to further review and validate these decisions.

It is important that the treating neurologist draws on the most robust evidence available on disease-modifying therapies for the long-term efficacy and safety of the therapeutic strategy.
In general, continued research, development and application of therapeutic strategies will reduce the cost of treating MS to improve access to treatment, especially in countries with lower healthcare budgets.
Overview of the key recommendations
Consult the strongest possible evidence base and generate further evidence to make good decisions about treatment and management strategies for MS.

Three key recommendations for change

The aim of MS Brain Health. Time Matters
Our vision is to create a better future for people with MS and their families.
Reproduced from Brain health: time matters in multiple sclerosis, Giovannoni G et al. Mult Scler Relat Disord 2016;9 Suppl 1:S5–S48, with permission from Oxford PharmaGenesis Ltd.
I have tried to make my contribution by reproducing and simplifying the key messages so that you can make better informed decisions and live with MS.
You can find out more about MS Brain Health at www.msbrainhealth.org.
See you soon and try to make the best out of your life,
Nele
For more information and positive thoughts, subscribe to my newsletter for free.
Click here for an overview of all podcast episodes published so far.
And at many more places.
* This text contains affiliate links. This means that I get a small compensation if you buy the product recommended by me through the link. For you nothing changes in the price of the product. And it helps me to pay for the blog and to write new posts.










