Dr. Barry Singer provides insights and perspectives into the precision medicine of today for people with multiple sclerosis. He also provides some outlook into future treatment options to come. Barry is a leading MS expert, who is steadily involved in clinical trials. He has experienced big changes in MS treatment over the years and is more than happy to offer his patients a variety of options to stop the find the best matching treatment for each of them.
Enjoy the interview and check out his website and podcast „MS Living Well“ where you can find lots of information on how to live well despite having multiple sclerosis.
Klicken Sie auf den unteren Button, um den Podcast zu laden.
Table of Contents
Introduction – Who is Dr. Barry Singer?
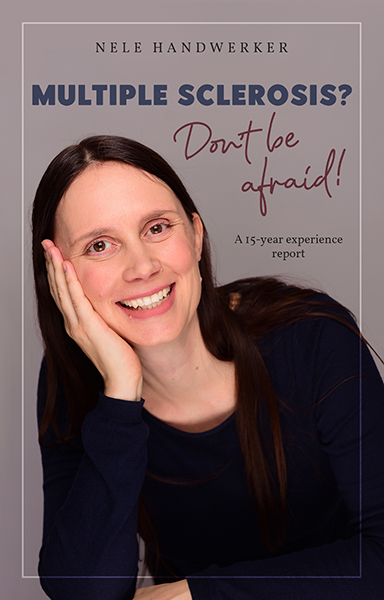
00:00:00] Nele Handwerker: Hello, Barry. It’s a pleasure to have you on the show and a warm welcome to St. Louis in the United States.
[00:00:06] Barry Singer: Well, thank you, Nele. Thank you very much for having me on your podcast.
[00:00:10] Nele Handwerker: And before we start with the podcast, it would be lovely if you could introduce yourself to the audience, to the few ones who don’t know you yet.
[00:00:17] Barry Singer: Ah, so yeah, so I am a director of an MS center here in St. Louis, in the heartland of the United States, right in the center. And I run a comprehensive MS center. We take care of over 4,000 patients at our center and do it with a whole team of wonderful nurses and medical assistants. And in addition, we do a lot of clinical research. So we’ve been involved in numerous clinical trials, bringing some of the medications that we have available to the market and research on remyelination. So very exciting research as well. And, you know, in my spare time, I have a website, MS Living Well, that was started in 2008, which provides comprehensive education for people living with MS around the globe. And then also MS Living Well podcast for the past five years. So keeps me busy.
[00:01:17] Nele Handwerker: Absolutely. And it’s really a great podcast. So I can just emphasize it’s really worth hearing into it. It’s a great one.

Current treatment landscape for MS
What are currently the most important treatment approaches for multiple sclerosis patients?
[00:01:38] Barry Singer: Well, there’s been a paradigm shift. I think, you know, for a long time, we started with maybe some of the safer medications that have been around for a long time and then escalate. So if you’re not doing well, you have some breakthrough disease and you go to a drug and maybe have a little more risk, but, you know, potentially getting better disease control. And what we find now, when we have so many highly efficacious medications out there, is that we can start with highly a effective drug and prevent a lot of the disability, so that people can live their best lives without disability.
So in the United States, what that means is we’re using a lot of monoclonal antibody treatment. And so we have approximately about 40% of people in the US who are taking B hyphen… Have B-cell depleting medications. So we see a tremendous amount of patients that are on these medications that kind of prevent recurrent relapses, new MRI activity. So I think that’s a real shift. We’re really just kind of pouncing on the treatment of the disease, from the very beginning to really change the disease course for people living with MS.
[00:02:52] Nele Handwerker: Yeah, absolutely. And I just saw numbers. We had here the MS Advent Symposium by Tjalf and he showed some numbers from Germany, the treatments we are starting off with and I think it’s just something like 20% monoclonal antibodies and you start off with more than 50% or something like that. I don’t remember the numbers correctly. Maybe you can correct me there, but at least we are going in the same direction. We are just starting at a much lower level with the highly effective therapies at the beginning.
[00:03:27] Barry Singer: Yeah, I think, you know, one of the exciting things, as you can see, if you get started on a very effective medication early on, you know, you just prevent having relapse after relapse and significant disability. Many of our medications now, like some of these highly effective drugs, are equivalent to having one relapse every 10 years, which is like amazing. You know, back in the day, you know, I’ve been around for a long time in the world of MS. We had only the injectable medications, the interferons and the tumor acetate. And people would sometimes have a relapse every couple of years on those medications and end up with significant disability later in life. And the poor people that, you know, before we even had it available, the people in their 70s, you know, some of these people were just really beaten up by MS. And so, I can already see it. Each generation does much better than the generation before, because of the therapeutic breakthroughs.
Personalized treatment of multiple sclerosis
Can you explain the role of precision medicine in the individualized treatment of MS patients?
[00:04:43] Barry Singer: Yeah, so when we think about personalized treatment, we’re really trying to match the right treatment for the right patient. And so we have a whole array of treatment options out there. So in the United States, we have over 20 FDA approved treatments. So it’s really trying to pick the right treatment for the right individual. And so personalized treatment really allows us to individualize, matching the right treatment for the right patient. You know, when we think about precision medicine, it’s kind of the same thing as personalized, but I kind of like the term personalized better, because we don’t have all the biomarkers, all the tools to definitely know this is the right treatment for the right patient. But there are a lot of factors that help us tailor that decision.
How do you create personalized treatment plans for your patients and monitor their success?
[00:05:38] Barry Singer: So one of the things that we need to do is, first of all, look at the disease activity in the individual that we’re working with. So if a patient comes in and they have highly active disease, a number of active lesions on the brain, a number of spinal cord lesions, we know we’re going to need to take a medication that has higher power to control that person’s individual disease. So that becomes very important that we match the right treatment to the amount of disease. Some people, on the other hand, may only have two or three small little spots in the brain and positive spinal fluid and they have very mild disease, so they may not necessarily need a medication that depletes part of their immune system long-term. So, I think part of it is understanding the amount of disease and that means looking at the spinal cord and the brain.
The other thing that we look at are there are certain risk factors for worse prognosis. So, incomplete recovery from the first attack. So, let’s say you had visual loss out of one eye and your vision never recovered completely, that would be an issue. The other things that we look for are men tend to do worse. And so men who are people that are older at the onset of the disease, like people age 40 and over, have a higher risk of progressive disability. So we want to look at those demographic features, the features of the individual, to make sure that we’re matching the treatment to their disease. Another important, oh, go ahead.
[00:07:11] Nele Handwerker: No, yeah, absolutely. And they were talking about it at ECTRIMS that it’s really important to see when the immune system is changing that you are balancing it with the right medication, right?
[00:07:23] Barry Singer: Right. So you got to pick the right, you know, the right amount of power for the disease. And then we really have to start tailoring our treatment to that individual. And so we have to look at a number of factors. One of the things that we… That’s very, very important is looking at other medical problems. And so that will help us make a decision. So for example, many of our people living with multiple sclerosis have other autoimmune diseases. So they may have rheumatoid arthritis, they may have inflammatory bowel disease, which is also colitis or Crohn’s disease, psoriasis. And so, some of our medications may help both.
We have some medications, for example, in the United States, we have Ozanimod, which is approved for all ulcerative colitis and for multiple sclerosis. And dimethyl fumarate, for example, was actually used for psoriasis in Germany before being used in the world of MS. So, a lot of times that becomes important. We also have to look at, you know, precision medicine or personalized medicine also has to look in the account if you have a history of cancer. Many patients over time develop cancer, whether it be breast cancer, skin cancer. So trying to pick the right medication for that individual is important. Some of our medications have been associated maybe potentially with a higher risk of certain types of cancer. So we have to really look at that individual.
The other thing is some of our medications, for example, terra flutamide, S1P medications can sometimes increase blood pressure. And so we also want to keep that in mind while we’re picking a medication for someone with hypertension. And the S1P medications like fingolimod… S1P medications like fingolimod can sometimes cause macular edema, particularly in patients with diabetes or uveitis. So again, these are some medical conditions that help navigate one way or another with medications.
What test results do you need for this, e.g. biomarkers?
[00:09:46] Barry Singer: Yes, Nele. So when we think about biomarkers, it’s basically a blood test to monitor disease. So when you think about people with diabetes, you can measure hemoglobin A1c. Or if you have monitoring cholesterol levels, you can check that in a blood test. So we’re now doing blood tests to look at multiple sclerosis disease activity. And we have one test that I’ve been using in the clinic for the past year. It is from a company called Octave and what we do is look at a panel of biomarkers, blood tests. Some include something called neurofilament light. Neurofilament lights in neurons and when neurons are damaged, this goes up in the spinal fluid and also up in the blood and we can actually measure it. So it’s damage to the nervous system.
And then we also have biomarkers that look at inflammation, biomarkers that look at myelin, the coding of the nerves and look for damage there. So we can use these panels that are associated with a risk of having increased disease activity. So let’s say, I put someone on a medication, it’s moderately effective, not the most effective medication, but good safety profile and then I could do a blood test on a patient and find out if they’re at high risk for new activity, or if they’re doing well in that treatment. Some people don’t want to go on MS treatments. You know, they just say, I’m not going to do it. I’m going to do diet, exercise. I’m not going to take a medication.
But if I do a blood test and it comes back high, maybe they might engage that conversation. Or someone later in life who says, do I really need this medication? So we’re starting to implement it. It’s definitely approved and available in the United States, but it’s a learning curve, but we’re starting to implement it. I do see very high levels in patients that do have very high activity, a baseline and before they start their disease modifying therapy. And so then once we initiate the DMT, the disease modifying therapy, we can see, how well they respond on the biomarker testing.
To what extent can predictive models help to determine the most effective treatment strategies for individual MS patients? And what are the current limitations, as I guess we are not yet there fully, aren't we?
[00:12:09] Barry Singer: Yeah, I don’t think we’re there yet. So I wish, I had a nice predictive model, where I can put in some information and get that info. Actually, I had Professor Jeff Simpson, Dr. Simpson on on my podcast talking about digital health. And he talked about a digital twin. So we could actually create a digital twin. And then we could do an analysis on that. And So, kind of predicting how someone would do and which disease modifying therapy would give that person the best option of doing well long-term. So, we’re not quite there yet. Hopefully, some artificial intelligence will help in that endeavor that will be able to analyze how other people have done globally on various disease modifying therapies to help guide our decision-making.
[00:12:59] Nele Handwerker: Yes, the digital twin is really a very interesting concept and I’m really looking forward to when this is all in place and working.
Can you share a success story where precision medicine has significantly influenced the outcome of an MS patient?
[00:13:14] Barry Singer: Yeah, so, well, in the United States, we’ve got a lot of privacy laws, but I can talk about some of our positive outcomes. I mean, I think where it really comes in handy is, if you have patients that have been on a disease-modifying therapy, not doing well and how do you get to the next agent? You know, where do you go? And so, I think this really… Becomes part of the comprehensive care. I think it also helps if you have an MS specialist with you, in this journey, to try to make the right decisions.
But sitting down and really analyzing, you know, what medications they’ve taken before, what kind of response that they had and if they weren’t doing well, you know, why weren’t they doing well? Is it new active enhancing lesions? Is it slow progression over time? And then trying to figure out, which medication has a strong chance of changing that disease course. Some of our medications have shown some benefit in progressive disease. We need better medications for progressive disease, but some have shown some benefit. And so if a patient’s going down that trajectory, then we may want to use a medication along that lines.
Someone’s having worsening cognition. We have some medications that have some data that support trying to prevent cognitive decline. And then again, we have to look at the patient’s medical history, you know, what kind of medical problems they have, how the medication is given. Some patients are very adherent to their medications and some people aren’t. I just had someone in yesterday, a terrible relapse, because they were not taking their medication regularly, as recommended. And so we have to find something that the patient feels comfortable with, they can take it and is able to, we call it here, stick with the plan over time.
To what extent do patients with progressive MS also benefit from the possibilities of precision medicine?
[00:15:34] Barry Singer: Yeah, I mean, I think the best way to prevent progression is by preventing the disease up front. And so I think if we can really get on top of relapsing MS early in the disease course, we can prevent more and more patients from becoming secondary progressive. And we’ve seen that over time with the implementation of disease modifying therapies, the time to secondary progressive has been delayed. And we’re trying to prevent more and more people from becoming progressive. But we do need new medications. So precision medicine or personalized medicine can say, okay, you got progressive disease, let’s try to pick a therapy that’s going to work best for you. But unfortunately, we don’t have enough tools or medications that really slow down slowly progressive disease. And so hopefully we’ll have more of those. I’ve been involved in clinical trials on this front and we’re hoping that there will be a new generation of medications that will work in progressive MS.
[00:16:34] Nele Handwerker: Fantastic. And I know you are really everywhere. I mean, I saw some posts on LinkedIn that you’ve been to China, for example, to help MS specialists there, or maybe people, who want to become specialists. I’m not pretty sure about that.
Which MS patients currently have access to precision medicine and how do you see it developing over the next 5 to 10 years?
[00:17:03] Barry Singer: Yeah, I think there’s definitely been a push for global access to disease-modifying therapies and clearly there’s inequality and inequities out there in the world, in terms of access to DMT. We did see the World Health Organization put three disease-modifying therapies on their list of essential medications. And I think that’s really critical that we have access for patients living around the world with multiple sclerosis and we know it’s a global disease. And so, to do personalized medicine, you need options. And so, we definitely need access and ways that we can get medications to patients now. Some have gone generic, so the price has decreased. But actually, in some countries, the generics aren’t even available.
And so, we really have to get the medication available out there. And then, when you have options, that’s when personalized medicine can come into play, where we can really start looking at different groups of patients and figuring out what responds. And it may not be the same. You know, a lot of our studies, you have to be careful, some of our studies have actually been done. Some trials are all in Europe, you know, and it’s frankly in Eastern Europe, where access to disease-modifying therapies may not be as good and people are willing to enroll in a clinical trial, where you have access to medication. And so we want to look at all different types of populations, like you mentioned the Chinese, you know, how does it respond in Asian populations, medications. So a precision medicine may be different for someone with a different ethnic background, different genetic background.
Patient involvement
How do you involve patients in decision making regarding their treatment plans?
[00:18:54] Barry Singer: So that’s really critical, Nele. I mean, we really want patients involved in the process of selecting the disease-modifying therapy and, you know, kind of, it’s your brain, it’s your spinal cord, let’s get you involved. And we call it shared decision-making. So it’s, you know, I think in traditional medicine, you know, the doctor says, this is what you should be on and writes a script and hands it to you. But a lot of times the patients never fill that script, you know, especially if they didn’t have a good relationship with the provider, the neurologist.
And so, what I like to do is sit down and go through someone’s history, their story, look at their… Do an examination, look at their MRI together, you know, we look at the pictures, so they understand what we’re trying to prevent, you know, lesions in the brain, lesions in the spinal cord, prevent brain shrinkage over time. And once they get on board, then it’s about sitting down and talking about treatments. So, you know, obviously, you know, if you’re an MS specialist, you’ve been doing this for a lot of years and you understand the pros and cons and nuances of what might be appropriate for an individual patient.
But then I like to circle back with maybe two or three options that I think might be appropriate and then go through the pros and cons of these medications. What are the benefits? What are the serious risks? What about day-to-day side effects? How is the medication given? And so, it’s really great to sit down and talk about all the nuances of the medication. And then we try to make a decision together. Sometimes, you know, someone’s not ready to make a decision right there on the spot and they may take some literature home, or I give them information from my MS Living Well website, which has all the different therapies and they can kind of read about them. And so that can be really, really, really great.
There is also the Ultimate Treatment Guide through the Multiple Sclerosis Association of America, which has good online resources, where you can compare medications and see videos of neurologists talking about the medications as well as people that are taking them. So, I think sometimes that helps. But I think you really should be part of that discussion. I think if you are helping to decide on the treatment, I think you’re going to be much more likely to not only stick with the medication, take the medication regularly, but also get the blood tests that are important to monitor the safety or what other safety testing needs to be done, you’ll understand why we’re doing this.
[00:21:31] Nele Handwerker: Absolutely. I always sat together with my neurologist and he explained to me, why the type of medication I’m taking is good for me and why it is working. And that’s why I have a really high therapy adherence and was maybe just for my birthday or so, not taking the daily medication. As you said, it’s my life, it’s my brain and my spinal cord and I have to take care of it and he is the expert who can give me in-depth knowledge and provide me with his expert view and recommendation.
[00:22:05] Barry Singer: Well it’s very, very important you can’t personalize treatment unless you understand, you get feedback from the patient. S when we have follow up appointments that’s what the importance of follow up appointments are, how’s it going, you know, how are you doing with your medication. Are you having day to day side effects, are you having diarrhea, are you having hair thinning, are you having, you know, what are the side effects that you’re having with the medication? Then we talk about, you know, ways to manage it.
You know, we did this a lot back in the day with interferon, which had flu like symptoms and achiness. Some people have injection site reactions. So, ways to kind of tweak the side effects are important. But if it’s intolerable and you know, you’re miserable on the medication, there’s no point in continuing. We have lots of different options. So, I think that’s part of the process, is really listening.
And then we also have to clearly monitor the disease. So, if you have new MRI activity, You’re having cognitive worsening, one of the things I do in my exam rooms on a regular basis is I have an ipad and it’s a cognitive testing. And you match symbols with numbers on an ipad, it just takes a couple minutes to perform and then I can find out how you’re doing compared to other people that are your same age, same educational background, without a mess and then come out of that over time. And if you’re losing ground, then we start to worry. Maybe we need to switch things up. So it’s another way of personalizing treatment.
[00:23:36] Nele Handwerker: Absolutely. And I’m doing this in my MS center as well. And I’m also doing brain training, NeuroNation. I don’t know if it’s international already, but they started it in Germany.
[00:23:45] Barry Singer: Sounds good, way to go.
[00:23:48] Nele Handwerker: Yes and it’s fun. I mean, they made it really playful. So that’s a good thing.
How do you educate MS patients about precision medicine and its potential impact on their treatment?
[00:23:59] Barry Singer: Yeah. So I think it’s really about, yeah, when I talk to patients, it’s not as much about precision medicine, it’s really about personalizing their care. And so it’s really about diving into understanding, who they are as an individual. What are their goals? What are their aspirations? How much risk are they willing to accept to achieve those goals? Some people don’t like medications with serious risks. That makes them very anxious. But kind of explaining, how we can control your disease and what the best approach is, I think, is very, very important. So it’s an ongoing conversation with the patients, to understand that we are trying to achieve the best outcomes. And so they understand, like why I’m doing the cognitive testing, why we’re doing biomarker testing and what we’re trying to achieve.
Emerging therapies
Are there promising new therapies or treatments for multiple sclerosis?
[00:25:05] Barry Singer: Yeah, so the biggest class of medications that we’re kind of excited about is BTK inhibitors. And so there’s some clinical research going on for this. We actually just got the type line results on ibrutinib, which ended up having about the same annualized relapse rate, the same rate as terra flutamide, also known as Obagio. And so, the first one that came out, at least in relapsing MS, looked about the same as terra flutamide. Frankly, the patients had very few relapses on both treatments. So, it was equivalent to about one relapse every seven to nine years.
So, the annualized relapse rate was very low, somewhere between 0.11 and 0.15 in the two trials. So, that was a very low amount of relapses. But the big question is really, can it slow down the progression? And so I think that’s the bigger question and that’s still pending. And so hopefully, this class of medication did work in progressive MS, because that’s really the unmet need. And the reason is, because these medications affect a cell, not only B cells, like many of our MS medications, but also affects a cell called microglia that are in the brain and seem to be driving chronic inflammation in the nervous system.
[00:26:28] Nele Handwerker: Okay. So do you have an idea when this, let’s say, more in-depth knowledge will be shared with the audience? Will it take two more years, three more years, four more years, when they can really say something about the neurodegeneration?
[00:26:44] Barry Singer: Well, I think that we may have some more data on progressive MS hopefully later this year, I think, we should have, yeah, hopefully, hopefully by the end of… The end of this year will have some more information.
[00:26:59] Nele Handwerker: That sounds good great.
[00:27:00] Barry Singer: We need more options.
[00:27:01] Nele Handwerker: Absolutely, absolutely. And I think, yeah, for relapsing, remitting, we have already quite some options. If it would really target the chronic inflammation, that would be great. And that’s what I hope for and I think many other people.
What breakthroughs or advances do you hope to see?
[00:27:21] Barry Singer: Well, I really would like a remyelinating compound. So, I’ve done five clinical trials at my center on remyelination, including phase one and phase two clinical trials. And so, that’s what I really like. I got a lot of patients that I’d like to fix, a lot of long-term patients that, you know, some of my patients I’ve known, frankly, for 24 years. And so, there are many patients that I would like to improve their quality of life and at least prevent the disease from getting worse. And so we really need remyelinating compounds.
I’ve done some trials with antibody therapies, but antibodies don’t tend to get… These monoclonal antibodies tend not to get into the brain and spinal cord. They tend not to get across the blood brain barrier, we call it, the membrane to get into the nervous system well. And not in high concentration. So we may need a compound that can, like a small molecule that can get into the brain and spinal cord and turn on remyelination.
We know about five to eight percent of the cells in the nervous system are immature myelin-making cells called oligos. They’re oligo precursor cells. And these cells are just hanging out. And so I’d like to turn them on and start making some new myelin. So anybody out there listening, who’s got a myelin compound that wants to bring in a clinical trial, I’ve got plenty of patients ready to go.
[00:28:50] Nele Handwerker: Yes. Yes, that would be so lovely. I had some interview guests here, who are working on this topic. It would be such a great thing to see.
Telemedicine and remote monitoring
How has telemedicine and remote monitoring for MS patients evolved in the context of precision medicine?
Nele Handwerker: As you are in the US, I mean, there are sometimes very faraway distances. I mean, my cousin lives in Texas and when she sees her parents-in-law, it’s like a nine-hour drive. So telemedicine is something interesting. Not so much in Germany, but there are lots of countries out there, where telemedicine is something interesting.
[00:29:23] Barry Singer: Yeah, so I think it has really changed the landscape, particularly with COVID-19. So COVID-19 really just blew it up, because for a while, there was a period of time where we were only virtual, because we were so afraid of our patients contracting the virus and being immunosuppressed. So, it’s definitely come a long way. So, we use telemedicine on a regular basis. Now, I think most people would rather just come into the office and be examined thoroughly. But, you know, I do have a lot of patients that live far away. We are in the central part of the United States and you know, out here in the heartland.
Many of my patients drive four hours one way for an appointment. So they’ll come in, be seen and 30 minutes later, they’re back driving home. So it’s a long way to go to see a specialist. And so sometimes every other appointment will do it virtually, to make it more convenient, particularly people that are fairly stable in terms of their disease. And their exam’s been pretty stable, then that’s a way of doing it. I think it also, you know, a lot of rural patients unfortunately get under treated in the United States. And so, you know, they may have a local neurologist, who does everything a general neurologist and it’s hard to stay up on MS with, you know, how can you do precision medicine, when there’s, you know, there’s 20 treatments and you’re taking care of every neurologic disease.
It’s an overwhelming amount of information to stay up on all the MS treatments as well. So, you know, a lot of the general neurologists tend to fall back on, you know, the few medications that they tend to use the most and are more comfortable with. So what telemedicine allows us to do is, connect some of these patients to an MS center, where we can really give them that personalized approach to picking disease-modifying therapy to match their disease.
[00:31:30] Nele Handwerker: Yeah. And it’s the same issue here in Germany, even though we are not such a widespread country. But yeah, when you are somewhere in a rural area, you go to a normal neurologist and of course they take care of a lot of stroke patients or dementia or all that. That’s an issue.
What opportunities and challenges do you see in this area?
[00:31:53] Barry Singer: One of the issues that we have in the United States is you have to be licensed by state. So during the pandemic, there was some emergency authorization. So I actually had, I actually had the ability to see my patients virtually there in California, I have patients actually all over the country and some people fly in for appointments. And so we were able to do a lot of this stuff virtually. But now that’s kind of shut down. So I’m in the process of getting a state license for Illinois and Missouri. And so you have to kind of go through this whole formal process to get licensure across state lines in the United States. So I think that’s a limitation.
Exams are a little bit of a limitation as well, you know, it’s hard to check reflexes over the internet. I have been able to do, you know, quite a few interesting exams. I have patients put their phone against the floor, on the wall, against the wall, so I can see people walk. And they can do heel to shin and finger to nose testing. You know, so I figured out creative ways to get a lot of information from the exam virtually, but it’s not the same thing as being able to really check someone out, to see if their legs have gotten weaker over time.
[00:33:08] Nele Handwerker: Yes. But it’s already lots of creativity, so that’s good. And I mean, I was at the same neurologist since the end of 2008 and I moved here last year. So from 2008 until 2022, I was going at least 200 kilometers, which is not much in United States distance proportions, but yeah, I think, if you have a good specialist, it’s totally worth it going there. And for some people, it’s nice if you can every now and then do something.
[00:33:40] Barry Singer: I think virtually, I think the one interesting thing is, I mean, you can definitely look at the MRIs, it’s the same. The conversation is the same. We can manage a lot of symptoms of MS is really a discussion more than anything else, in terms of how you’re going to manage fatigue and bladder dysfunction and nerve pain. So some of this, you don’t really need to be in person to do some of this. So and for some people it’s more comfortable to be at home. You actually get a little insight. You know, some of my patients are, you see a cow in their backyard and other people are in a more urban situation, with lots of family and this very small apartment. And so you get to see, you know, some of the natural environment and of course you get a little more context to understand how the patients are doing in their journey with ms.
Farewell
How and where can interested people follow your research activities?
[00:34:44] Barry Singer: Yeah, so definitely, you know, if you are interested, check out the MS Living Well podcast. So it’s on various podcast apps, including Apple Podcasts. The website is MSLivingWell.org. And so a lot of great information there, there’s a blog, there is information on understanding your disease, I got animated videos, understanding your MRI, and some award-winning content there. And then I’m on Twitter, or X, I guess it’s called now. And so, you know, I post there as well, particularly during the meetings, the academic meetings, like Ekram’s and Actrooms and try to post the latest news. So if something new is going on in the world of MS, I put it out there and I announced my podcast on there as well.
[00:35:41] Nele Handwerker: Fantastic. Yes. And I will link all of these in the show notes. And I met you at ECTRIMS in Milan. Next year, I don’t know, because I am pregnant as of now, so I don’t know. It will be half a year old, so probably I won’t join Copenhagen, but let’s see.
[00:36:00] Barry Singer: Maybe virtually.
[00:36:01] Nele Handwerker: Maybe for joy and maybe I will go to a few sessions, if the baby is lovely and friendly and sleeps a lot. But yeah, Barry, thank you very much. Thank you very much for everything you do. Thank you very much for taking your time for the interview. It was a pleasure. And I will check out on all your information and I think it will be very interesting to lots of the listeners. And yeah, thanks.
[00:36:24] Barry Singer: All right. Thank you, Nele, for the opportunity to be on the podcast.
[00:36:28] Nele Handwerker: Bye-bye. Bye-bye.
Links to Dr. Barry Singer’s online presence:
- MS Living Well Website: https://www.mslivingwell.org/
- MS Living Well Blog & Podcast: https://www.mslivingwell.org/blog/
- X or Twitter: https://twitter.com/drbarrysinger
See you soon and try to make the best out of your life,
Nele
For more information and positive thoughts, subscribe to my newsletter for free.
Click here for an overview of all podcast episodes published so far.
And at many more places.
* This text contains affiliate links. This means that I get a small compensation if you buy the product recommended by me through the link. For you nothing changes in the price of the product. And it helps me to pay for the blog and to write new posts.










